Author: Tim Perry
A debate hosted by IQ2, The US Health Care System Is Terminally Broken, inspired this article. The debaters were all knowledgeable and experienced in the current US “health care” system, including CEOs of major hospital systems. However, I was simply amazed by how poorly the debate went even though everyone agreed “health care” is broken. If nothing else, this debate helped me understand that we discuss “health care” only in the context of clinical care, with just a passing glance at what goes on outside the clinic. We need to develop an appreciation for both Acute and Chronic Care.
The Right Model
“The US Health Care System Is Terminally Broken” is the wrong premise for the debate we need. If we must stay with a health care metaphor, let it be “The US Health Care System Has Delivered Twins: Acute and Chronic Care”. These are two similar yet separate entities and we need to nurture them as such.
While watching the debate I realized three things:
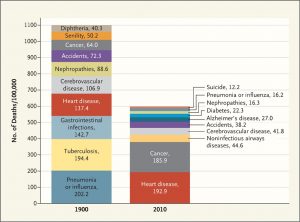
1) Acute Care (or “sick care” or “disease management”) actually works quite well for what it was designed to do: address infectious diseases and trauma that were the leading causes of death at the turn of the 20th Century (early 1900’s).
2) People, even the experts, still equate “health care” with clinical acute care.
3) Chronic Care is pretty well just seen as Acute Care over a longer period of time, with little appreciation for and action on non-clinical determinants (the so-called Social Determinants) of health or complementary therapies that better address chronic illnesses.
Could it be that we have done so well with “acute care” that we assume all health issues are treated best with the same acute care model? In terms of our debate metaphor we want to focus on one child when we really have two.
Acute and Chronic Care
Thomas Sydenham, known as the “father of English medicine”, wrote about the difference between acute diseases and chronic diseases in the 17th century. Essentially, he saw acute diseases as those outside human control (e.g., infections, trauma) while chronic diseases are rooted in poor lifestyle decisions (e.g., diet, drinking, etc.).
Dividing diseases into acute and chronic is an old medical device. The English physician Thomas Sydenham (1624–89) differentiated “Acute [diseases] meaning those of which God is the author, chronic meaning those that originate in ourselves”. Mutatis mutandis, Sydenham’s dictum, is a summary of modern medicine, with chronic diseases defining everything else by exclusion.
Source: http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(15)60007-1.pdf
And the world of Modern Medicine has done a good job with acute diseases, nearly eradicating many of the leading causes of death from the early 1900s like pneumonia, tuberculosis, and, gastrointestinal infections. These acute diseases still present dangers in the US (a particularly lethal flu outbreak is underway while I write this article) and the rest of the world. However, the acute illnesses of the turn of the 20th century have largely been replaced in the US by the chronic diseases of the 21st century: heart disease, cancer, COPD, diabetes, etc.
Source: http://www.nejm.org/doi/full/10.1056/NEJMp1113569
Of course, all mortals have a finite time on this planet. There will always be some leading cause of death. Chronic illnesses are not only are the leading causes of death but also preventable deaths, poor quality of life and constitute more than 80% of our “health care” costs. It is time to fix this with both Acute and Chronic Care.
A “health care” system should be more than avoiding death and injury. As the World Health Organization defines it “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”
Acute Care has arguably done well historically in the “absence of disease or infirmity” department but has been sorely lacking in “complete physical, mental and social well-being”. We need a new approach with both Acute and Chronic Care.
More Efficiently Delivering The Wrong Thing
Stated bluntly, Acute Care cannot fix chronic illnesses that are rooted in socio-economics and poor lifestyle decisions. If we double the number of hospitals it will not stop obesity as long as Americans continue to make poor nutrition choices. After we wring out the last ounce of waste in pharmaceuticals there will still be no prescription for loneliness, potentially a bigger risk than obesity or smoking.
Yet this message does not sink in with decision makers in the the US “health care” system. Where we need to offer more complementary services to address obesity, addiction, loneliness, etc. we get drug store chains buying insurance companies to optimize costs. Where we need more primary care, we get hospitals acquiring primary care practices… only to overextend and need a round of hospital mergers to rationalize cost structures. The US “health care” system is fixated on improving Acute Care efficiency to address problems completely outside its capabilities while ignoring innovative and holistic approaches to so many chronic illnesses and well-being.
The recently announced Amazon, Berkshire Hathaway, and JPMorgan Chase partnership to improve health and cuts costs for their employees has put even the most ardent defenders of the acute care status quo on notice.
Missing Completely What Is Broken
Borrowing from one of my previous articles:
- The US spent $3.2 TRILLION on “health care” in 2015 [source].
- The top 10 chronic illnesses had direct costs to payers of nearly $1.4 TRILLION [source] and even more indirect costs (e.g., lost productivity) as well as human suffering.
- 80% of chronic diseases are preventable with better Lifestyle decisions [source].
We have data that tell us how to prevent 80% of the diseases that consume nearly 50% of our “health care” expenditures and rob millions of Americans of quality of life and even Life itself. We know this. Right now. This very minute. But we do nothing to change. (Predictive Analytics– Wasted Resources in Current Health Care System)
The debate that inspired this article, The US Health Care System Is Terminally Broken, focused on hospitals, equipment, insurance, etc. That is where the money is. However, that is not where the value is. The value is in improving lives and saving lives that are threatened by chronic illnesses. That does not come from pills, surgeries, more hospital beds, more physician specialists or even cheaper “health care” bills. It comes from Chronic Care.
A real healthcare system, and not a “sick care” system, will promote a “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” A real healthcare system will recognize and reward both Acute and Chronic Care as distinct approaches that require different skills, time horizons, incentives, reimbursements, and outcome measures (yeah, we do need to start measuring and tracking outcomes and not just talk about them).
What does this mean? It means we must stop the focus on immediate fixes with acute care tools (prescriptions, surgeries, etc.) and embrace the human needs behind so many chronic illnesses that require different approaches to get at the root of these problems, not just the symptoms. It means Acute Care needs to roll over and share the bed with Chronic Care.
Be Well!
-Tim
Originally posted on LinkedIn: https://www.linkedin.com/pulse/twins-us-health-care-system-acute-chronic-tim/
Our Model