Rural America Is Short Mental Health Professionals
As the US and other countries integrate mental health as a critical component of overall health, we find rural America is critically short on mental health professionals. This is especially concerning with an opioid epidemic in many rural areas where mental health programs could make a considerable difference.
Almost every American will, at some point or another, face a mental health challenge. It may be related to depression, anxiety, suicidal thoughts, substance abuse or maybe something more circumstantial like grief over a loss or trouble adjusting to a life change. The CDC reports 43.4 million adults suffered from some sort of behavioral health issue in 2015 alone.
Now, imagine there wasn’t a psychiatrist or psychologist for miles around, let alone another specialist who these millions of people could trust with their specific needs. This is what life is like for many Americans in rural communities.
A new study in the American Journal of Preventive Medicine finds that a majority of non-metropolitan counties (65%) do not have a psychiatrist and almost half of non-metropolitan counties (47%) do not have a psychologist.
This is troubling because poor access to mental health care, according to experts, is a serious issue that overlaps with other public health crises like drug abuse and suicide.
Because of this, mental health care is often seen as a last resort instead of a preventative measure or an ongoing program of therapy. That can have devastating consequences, because the problem is only treated when it becomes a full-blown crisis.
“The services that are available become much more restricted,” Rainer says. “It becomes oriented towards crisis intervention, not prevention. It’s, let’s get rid of your crisis as it’s happening.’ And if you don’t have good insurance or enough money, that’s the best you can hope for.”
Practitioners are overwhelmed
Rainer says the frustrations for small-town care providers are endless. The web of mental health resources doesn’t just include psychiatrists and psychologists, but also external resources like shelters, hospitals and community support groups.
In small communities, those types of resources just aren’t there, and that leaves professionals shouldering a Herculean obligation.
“As a practitioner, I am asked to be the end of the road,” Rainer says. “For mental health, I would hope that I would be one piece of a larger puzzle to get people to an improved quality of life, not to be the last resource that they have available.”
For more information please see the original article: There’s a severe shortage of mental health professionals in rural areas . Here’s why that’s a serious problem – CNN
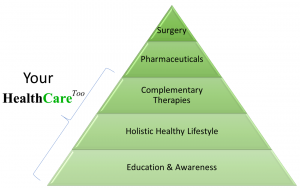
Our Model