About Health, Not Technology

So… quick question: is the US “health care” system a good process ready for silicon?
Security
Let’s start with some easy items. Security is the foundation. It is really hard to put in security measures after the fact. So what does security look like in the US “health care” system? In 1996 the Health Insurance Portability and Accountability Act (HIPAA) became law and has generated most of the rules for Protected Health Information. Since 2003 over 171,000 complaints have been filed that resulted in 53 cases with actual fines / settlements (totaling $75,229,182). That’s roughly 15 years. A week in any moderately-sized hospital system would reveal 53 violations. Security is not ready and not enforced. The on-going wave of ransomware attacks, breaches, hacks, etc. demonstrate this. As a comparison of regulatory oversight, the FDA issued over 500 Warning Letters just in 2017. 500 Warning Letters may (or may not) be too much but 53 HIPAA violations in 15 years in light of tens of millions of comprised medical records certainly does not reflect a serious approach to security or enforcement.
Health IT
In 2009 the Health Information Technology for Economic and Clinical Health (HITECH) promised to improve both “health care” and the economy by getting medical providers to use Electronic Medical Records in a meaningful way. The US Federal Government has paid roughly $36 Billion to the medical community for “meaningful use” of those Electronic Medical Records (or Electronic Health Records, if you like). Medical organizations have dumped billions more into rolling out these programs. Are physicians happy? No. Are patients happy? No. Is there reliable interoperability among all these systems? No.
So security is either not in place or not enforced. Physician and patient satisfaction are both low, especially considering the billions invested in Electronic Medical Records. Systems can share medical data only in the best of circumstances. At least the “health care” system produces uniform medical performance throughout the US… right? Also, No.
Disparities
There is, indeed, disparity in medical care within the US, as the Washington Post highlighted in Our infant mortality rate is a national embarrassment:
The U.S. rate of 6.1 infant deaths per 1,000 live births masks considerable state-level variation. If Alabama were a country, its rate of 8.7 infant deaths per 1,000 would place it slightly behind Lebanon in the world rankings. Mississippi, with its 9.6 deaths, would be somewhere between Botswana and Bahrain.
Medication does not become less effective when it crosses a state or county line. Physicians do not lose part of their training when they practice in a poverty-stricken zip code. Yet there is evidence of health disparities based on where people live, level of education, race, income, and so on. Technology has not and will not fix this.
Sick Care
“Health care” in the US is, unfortunately, “sick care” where “Doctors no longer minister to a distinctive person but concern themselves with fragmented, malfunctioning” body parts, as Dr. Lown wrote in “The Lost Art of Healing“. This is a broken system, one not worth putting into silicon… yet. We need change that is about health, not technology.
Improving Quality in Health
Rather than “siliconizing” a broken “sick care” system, we should endeavor to improve the system and quality first. There are efforts such as MACRA to do this but, let’s be honest, most people don’t even know what MACRA is. We need to approach this from the consumer’s point of view, not the Federal bureaucrat’s point of view. Right now, the best experience with “sick care” for a consumer is never to have an event that requires medical treatment.
Think about it. If a person came into this world, lived a long and healthy life, and passed into the next world without setting foot in a hospital… that person would be “lucky”. No one wants to be a patient in a “sick care” system… though most people are thankful that we have advanced medical capabilities for those times when we truly need them (e.g., accidents).
The Multi-Trillion Dollar Question
The US spends trillions of dollars annually on medical care, more per capita than any other nation. Yet the US has the worst outcomes among developed nations (and some lesser-developed nations). The question is not how to make a broken system more efficient (so bad things happen more quickly) but to fix the system itself… transform “sick care” into “healthcare”. We need change that is about health, not technology.
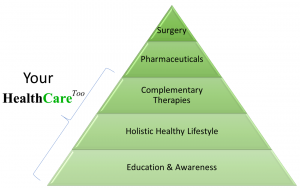
Putting more resources into early education (e.g., WholeHealthED), better nutrition, early intervention with less-invasive therapies, and more primary care interactions with less reliance on conventional medical approaches (e.g., pharmaceuticals and surgeries) will enhance consumer satisfaction and reduce costs. Consumers and some providers realize this and have already put more dollars to work.
Not A Technology Question
John Zachman, the father of IT Enterprise Architecture, once told me that technologies do not solve problems because the problems do not stem from technologies; problems stem from poorly-defined, poorly-understood, poorly-controlled processes (just look at Electronic Medical Record workflows for a textbook example). If we want to reduce costs and improve health then we must put resources on keeping people healthy and not simply making “sick care” more efficient with yet another set of technologies.
Will blockchain, virtual reality, Bitcoin, Ethereum, smart contracts, containers, smart devices, FHIR, 5G, Software Defined Networking, quantum computing, artificial intelligence, predictive data analytics, virtual assistants, self-driving cars, robots, drones, Internet of Things, or any of the coming technologies make people healthy? No more than the current crop of technologies: server blades, Storage Area Networks, cloud, virtual machines, 3G, 4G, WiFi, smart phones, Java, agile, Internet 2, social media, Electronic Medical Records, Hadoop, Big Data, among others. Technologies are simply tools, not solutions. Only when we focus technology, policies, and resources on keeping people healthy through better Lifestyle decisions, a holistic approach (body, mind, spirit), and addressing Social Determinants of Health can we improve health and reduce costs. We need change that is about health, not technology.
Be Well!
-Tim
Tim Perry, MPA, MS, CPHIMS, CISSP is the Chief Information Officer of Consumer Health platform HealthCareToo.com. Tim has a deep passion for transforming and improving healthcare that spans two decades. He is blessed with a wonderful wife and two inspiring children. Tim has practiced Tai Chi (Taiji Chuan) for over 15 years and enjoys cooking wholesome (and easy) meals.
Our Model